Unlocking the Secrets of Chlamydia: Your Comprehensive Guide to Protection, Treatment, and Empowerment
I. Introduction
Definition and Overview of Chlamydia
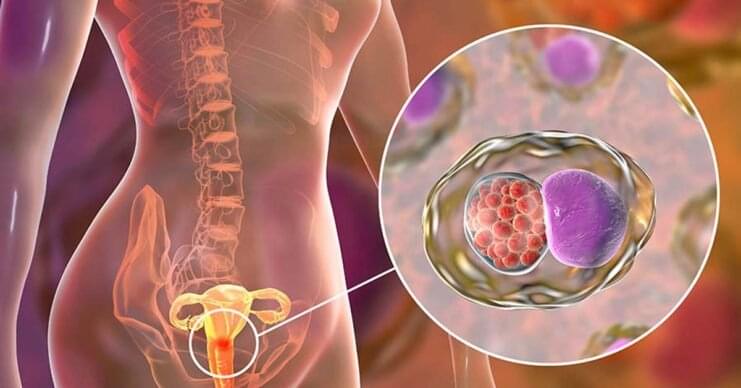
Let’s kick things off by unraveling the mystery of Chlamydia. It’s not just a tongue-twisting word; it’s a common sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis. Imagine Chlamydia as a tiny, sneaky intruder that can wreak havoc if left unchecked. But don’t worry; we’re here to arm you with knowledge.
Prevalence and Significance in Females
Ladies, pay attention because this one’s for you. Chlamydia has a soft spot for females. It’s like the unwanted guest that keeps showing up at the party. With millions of cases reported worldwide each year, its impact on women’s health is no joke.
Purpose and Scope of the Article
The mission is clear: we’re here to equip you with all the knowledge you need about Chlamydia. From what causes it and how it’s transmitted to the nitty-gritty of symptoms, diagnosis, treatment, and prevention, this article is your comprehensive guide.
II. Understanding Chlamydia
A. What is Chlamydia?
- Microorganism Responsible (Chlamydia trachomatis)
Think of Chlamydia trachomatis as the ringleader of this microbial circus. It’s a sneaky bacterium with a knack for causing trouble down below. Understanding its structure and behavior is the first step in the battle against this STI.
- Transmission Methods
Chlamydia is an equal-opportunity infection. It can be transmitted through sexual and non-sexual contact. So, whether you’re getting intimate or sharing a towel, be cautious. It’s a bacterium with no boundaries!
B. Signs and Symptoms
- Common Symptoms in Females
Ladies, if Chlamydia were a movie, its stars would be vaginal discharge, pelvic pain, and burning during urination. These are the telltale signs that something’s amiss down there. It’s like a red flag waving, telling you to seek help.
- Asymptomatic Cases
Now here’s the tricky part. Chlamydia can be a master of disguise. In many cases, it lurks silently without any noticeable symptoms. You might be thinking everything’s fine, but this silent invader can be quietly causing damage. Regular check-ups are your secret weapon against it.
C. Risk Factors
- Age and Sexual Activity
Age is just a number, but when it comes to Chlamydia, it matters. Younger individuals and sexually active adults are more susceptible. So, whether you’re 18 or 80, it’s crucial to stay informed.
- Multiple Sexual Partners
Variety might be the spice of life, but not when it comes to sexual partners. Having multiple partners increases the risk of Chlamydia transmission. Safe and monogamous relationships can be your shield.
- Lack of Barrier Protection
Think of condoms as your armor in the battle against Chlamydia. They’re not just for pregnancy prevention; they’re your defense against STIs, too. Don’t underestimate their power.
- Other Predisposing Factors
Chlamydia doesn’t discriminate. It can affect anyone, regardless of gender, race, or socioeconomic status. Other factors like weakened immune systems and co-existing STIs can also up the risk.
III. Chlamydia Diagnosis
A. Screening and Testing Methods
- Nucleic Acid Amplification Tests (NAATs)
If you’ve ever wondered how doctors catch Chlamydia, NAATs are their secret weapon. These tests are like detectives hunting down the DNA of the bacterium. They’re incredibly accurate, making early detection possible.
- Urine Tests
Imagine this: a simple urine sample can reveal whether you’re harboring Chlamydia. It’s convenient, painless, and highly effective. So, if you’re due for a check-up, don’t skip the pee cup!
- Vaginal Swabs
Sometimes, a urine test may not tell the whole story, especially for women. Vaginal swabs can provide more accurate results in such cases. It’s all about finding the right tool for the job.
B. Importance of Early Detection
The early bird catches the worm, and when it comes to Chlamydia, early detection can prevent a lot of trouble. Timely diagnosis is your ticket to effective treatment and fewer complications.
C. Challenges in Diagnosis
Sadly, the path to diagnosis isn’t always straightforward. Barriers like access to healthcare and the stigma surrounding STIs can make getting tested a challenge. But remember, knowledge is power, and there’s no shame in seeking help.
IV. Complications of Untreated Chlamydia
A. Pelvic Inflammatory Disease (PID)
PID is like the nightmare sequel to Chlamydia. If Chlamydia goes untreated, it can lead to PID, which can cause chronic pelvic pain and even infertility. Think of PID as Chlamydia’s evil sidekick, and you definitely want to avoid that duo.
B. Infertility and Ectopic Pregnancy
Untreated Chlamydia can have serious consequences, including infertility. It’s like a fertility thief in disguise. Plus, it raises the risk of ectopic pregnancy, a potentially life-threatening condition. Taking Chlamydia seriously is your best defense.
C. Other Reproductive Health Issues
Chlamydia isn’t a one-trick pony. It can also lead to conditions like endometritis and salpingitis, which can disrupt your reproductive health. It’s not a risk you want to take lightly.
D. Disseminated Chlamydia
In rare cases, Chlamydia can go on a road trip through your body, affecting organs beyond the genital area. This can lead to systemic infections and serious health issues. It’s like Chlamydia’s grand finale, and you want to avoid being in the audience.
V. Chlamydia Treatment and Management
A. Antibiotics for Chlamydia
- Commonly Prescribed Medications
Meet your Chlamydia-fighting superheroes: antibiotics. Drugs like azithromycin and doxycycline are often used to vanquish this bacterium. They work by disrupting its growth and reproduction.
- Treatment Regimen
Think of Chlamydia treatment as a well-choreographed dance. You’ll need to follow a specific regimen and complete the full course of antibiotics to ensure that you’ve truly defeated the infection.
B. Partner Notification and Treatment
Chlamydia can be a sneaky chain reaction. If you’re infected, it’s crucial to notify your sexual partners so they can get tested and treated. It’s a bit like superhero teamwork – everyone needs to do their part to save the day.
C. Follow-up and Retesting
Your journey with Chlamydia doesn’t end with antibiotics. After treatment, follow-up appointments and retesting are essential to confirm that the infection is gone. It’s like making sure the villain doesn’t come back for a sequel.
D. Avoiding Reinfection
Once you’ve beaten Chlamydia, you want to keep it at bay. Safer sexual practices, including condom use and regular testing, can help you stay infection-free.
E. Alternative and Complementary Therapies (If Applicable)
While antibiotics are the gold standard, some people explore alternative and complementary therapies. These can include natural remedies and supplements, but it’s essential to consult with a healthcare professional before going this route.
VI. Prevention of Chlamydia
A. Safe Sexual Practices
- Abstinence
Abstinence is the surefire way to avoid Chlamydia and other STIs. It’s like saying no to the party where the uninvited guest (Chlamydia) might show up.
- Condom Usage
Condoms are like your personal bodyguards. They provide an extra layer of protection against Chlamydia and other STIs. Plus, they’re easily accessible and user-friendly.
B. Vaccination (If Applicable)
While there’s no Chlamydia vaccine on the market yet, researchers are hard at work trying to develop one. Keep an eye on future developments, as a vaccine could be a game-changer in preventing Chlamydia.
C. Screening and Testing Recommendations
Knowing your Chlamydia status is crucial. Regular testing, especially if you’re sexually active or have multiple partners, can help you catch and treat the infection early.
D. Education and Awareness
Knowledge is power, and when it comes to Chlamydia, awareness is your best defense. Comprehensive sexual health education can empower you to make informed decisions and protect yourself.
VII. Chlamydia and Women’s Health
A. Impact on Reproductive Health
Chlamydia isn’t just a nuisance; it can have a profound impact on your reproductive health. It’s like a villain trying to steal your future family plans. Understanding this impact is crucial for taking the infection seriously.
B. Psychological and Emotional Aspects
A Chlamydia diagnosis can bring a whirlwind of emotions. It’s essential to address the psychological and emotional aspects of dealing with an STI, seek support, and remember that you’re not alone.
C. Reducing Stigma
The stigma surrounding STIs can be a major barrier to testing and treatment. Let’s work together to break down these barriers and create a world where seeking help for Chlamydia is met with understanding and compassion.
D. Access to Healthcare and Disparities
Access to healthcare should be a right, not a privilege. Unfortunately, disparities in access to Chlamydia screening and treatment persist, especially in underserved communities. It’s time to bridge these gaps and ensure that everyone has access to quality care.
VIII. Case Studies and Personal Experiences
A. Real-life Stories of Women Affected by Chlamydia
Sometimes, the best way to understand an issue is through personal stories. We’ll share real-life accounts of women who’ve faced Chlamydia, their journeys, challenges, and triumphs.
B. Lessons Learned and Insights
From these personal experiences, we can extract valuable lessons and insights. These stories serve as a reminder that Chlamydia can affect anyone, and there’s strength in sharing and supporting one another.
C. The Importance of Destigmatizing the Condition
Personal stories play a vital role in reducing the stigma around Chlamydia and STIs in general. By sharing these experiences, we contribute to a more open and accepting dialogue about sexual health.
IX. Research and Future Directions
A. Ongoing Studies and Breakthroughs
Researchers are hard at work, seeking new ways to combat Chlamydia. We’ll explore the latest studies and breakthroughs, shedding light on the promising developments in prevention and treatment.
B. Emerging Treatments and Prevention Strategies
Innovative approaches to Chlamydia prevention and treatment are on the horizon. Keep an eye out for new strategies that could revolutionize how we tackle this STI.
C. The Quest for a Chlamydia Vaccine
The holy grail of Chlamydia prevention is a vaccine. We’ll delve into the ongoing quest for a Chlamydia vaccine and the potential it holds for a Chlamydia-free future.
Conclusion
Let’s take a moment to recap what we’ve covered. From understanding Chlamydia to its diagnosis, treatment, prevention, and impact on women’s health, we’ve left no stone unturned.
Importance of Chlamydia Awareness
Knowledge is your best defense against Chlamydia. By raising awareness and destigmatizing the condition, we can empower individuals to take charge of their sexual health.
Encouragement for Regular Screening and Safe Practices
We’ll leave you with a strong message: regular screening, safe sexual practices, and open communication about sexual health are your tools for a Chlamydia-free future. Remember, you’ve got this!
Here are 10 frequently asked questions (FAQs) about Chlamydia:
1. What is Chlamydia, and how is it transmitted?
- Chlamydia is a sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis. It is primarily transmitted through sexual contact, including vaginal, anal, or oral sex, with an infected person.
2. What are the common symptoms of Chlamydia in females?
- Common symptoms in females may include vaginal discharge, pelvic pain, pain or discomfort during urination, and abdominal pain. However, it’s important to note that Chlamydia can also be asymptomatic, meaning some individuals may not show any noticeable symptoms.
3. How is Chlamydia diagnosed?
- Chlamydia is diagnosed through various methods, including nucleic acid amplification tests (NAATs), urine tests, and vaginal swabs. NAATs are considered the most accurate method for diagnosis.
4. What are the potential complications of untreated Chlamydia in females?
- Untreated Chlamydia can lead to serious complications such as pelvic inflammatory disease (PID), which can cause chronic pelvic pain and infertility. It also increases the risk of ectopic pregnancy and can affect other reproductive health aspects.
5. Is Chlamydia treatable, and what is the treatment regimen?
- Yes, Chlamydia is treatable with antibiotics. Commonly prescribed antibiotics include azithromycin and doxycycline. Treatment typically involves a short course of antibiotics, but it’s essential to complete the full treatment regimen as prescribed.
6. How can I prevent Chlamydia infection?
- Preventing Chlamydia involves practicing safe sexual behaviors, such as using condoms consistently and correctly, getting regular screenings if sexually active, and discussing sexual health with partners. Abstinence is the most effective way to prevent Chlamydia and other STIs.
7. Are there vaccines available for Chlamydia?
- Currently, there is no approved vaccine for Chlamydia. However, ongoing research aims to develop a Chlamydia vaccine in the future.
8. What should I do if I test positive for Chlamydia?
- If you test positive for Chlamydia, it’s crucial to follow your healthcare provider’s treatment recommendations, inform your sexual partners so they can get tested and treated, attend follow-up appointments, and practice safe sex to prevent reinfection.
9. How can we reduce the stigma surrounding Chlamydia and other STIs?
- Reducing stigma involves promoting open and non-judgmental discussions about sexual health, raising awareness about STIs, and emphasizing that anyone can contract them. Education and empathy are key to destigmatizing Chlamydia and other STIs.
10. Where can I find support and additional information about Chlamydia?
- You can find support and information from healthcare providers, sexual health clinics, and reputable organizations specializing in sexual health. Additionally, online resources and hotlines are available for confidential assistance and guidance related to Chlamydia and STIs.